Navigating Health with Peers
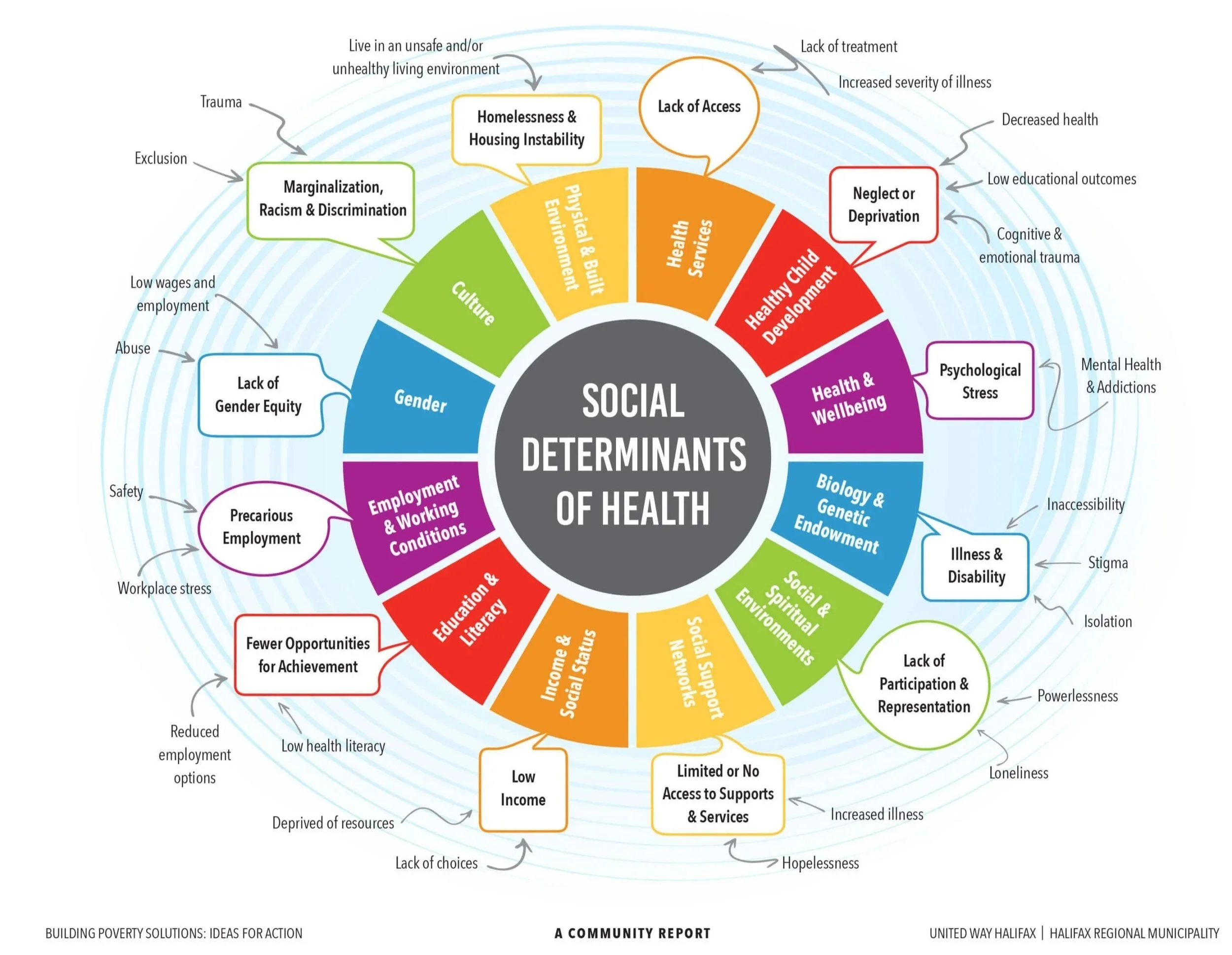
Health is about more than medical care. A person’s well-being develops from the dynamic interplay of their environment, experiences, and the support they receive, where stability in one aspect strengthens well-being while vulnerability in another area can threaten overall health. For people living with HIV and members of the transgender community, these factors are often marked by systemic inequities and discrimination.
To better understand and track our clients’ progress toward stability, Chicago House uses the Snohomish County Self-Sufficiency Matrix. This tool allows us to assess multiple dimensions of a client’s life—from housing to mental health to income—and to chart changes over time. Rather than reducing someone to a diagnosis, it highlights both vulnerabilities and strengths, guiding our staff in tailoring supports that move individuals closer to independence and long-term stability.
For years, Chicago House case managers were the primary guides for clients navigating care. As the complexity of client needs grew, it became clear that no single staff member could shoulder the entire responsibility. This insight led to the development of our Peer Health Navigation model in partnership with Dr. Lisa Razzano (UIC) and Dr. Patrick Corrigan (Illinois Institute of Technology). Thanks to funding from the Sylvia Fund of The Chicago Community Trust, we are now concluding the second year of implementation.
Peer Health Navigation brings trained peers—people with shared lived experience—into the care team. Disclosure, when chosen by the peer navigator, becomes a bridge to trust: it signals to clients that the person supporting them understands the realities of living with HIV or navigating systemic barriers firsthand. This trust has already shown powerful results: clients are attending appointments more regularly, following through with providers, and developing stronger relationships with their case managers.
The model also empowers our staff. By distributing responsibility across a team, case managers can focus on specialized services while peers handle daily guidance and connection. Through a “train-the-trainer” approach, we have begun scaling Peer Health Navigation across our housing programs, and with funding from the Public Health Institute of Metropolitan Chicago, we are expanding the model specifically within TransLife Care. This approach is now becoming an integral part of our organizational practice.
By centering lived experience in care, Chicago House is demonstrating how social factors shape health. As we expand housing services and prepare for a future where the majority of our clients will be over 50 and living with HIV, Peer Health Navigation offers stability and innovation through connection, which is often overlooked in traditional models. As we have learned to date, it helps individuals climb the self-sufficiency scale while reshaping the way we deliver dignified services.